Glute Medius Tendinopathy (lateral or pain on the outside of the hip)
Figure 1: Hip Pain - Hip Bursitis, Hip Tendonitis - Physio Frenchs Forest, Physio Macquarie Park
Do you have pain on the outside of your hip?
Have you been told you have bursitis of the hip?
Have you been told you have glute tendonitis?
First of all it’s important to understand what a tendon is:
Tendons are the collagenous bands of fibrous connective tissue that attach muscles to bones. The term tendinopathy is used to describe both the pain and associated cellular changes to a tendon that cannot tolerate the load under which it has been placed. Therefore, tendinopathies (tendonitis) are generally considered to be a load, or overuse, style of condition. Contrary to popular belief, tendinopathies (tendonitis) involves minimal inflammation at the site of pain.
What is glute med tendinopathy?
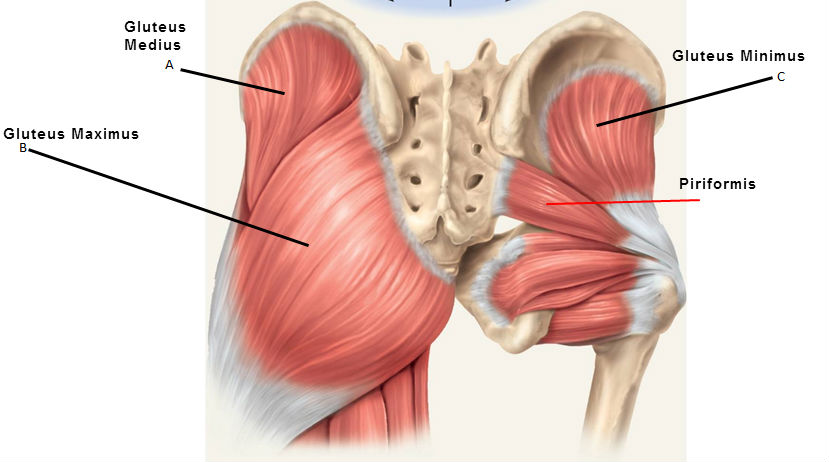
A tendinopathy that involves the gluteal muscles, and in particular a muscle called Gluteus Medius, is a common presentation in a variety of populations. These muscles start at varying points around the pelvis, and attach onto an area at the top of the femur. This group of muscles actively extend and externally rotate the lower limb at the hip joint.
In an effort to simplify diagnosis, gluteal tendinopathy is now classed under the umbrella term of Greater Trochanteric Pain Syndrome (GTPS), which includes other regional contributors to pain, such as the trochanteric bursa (bursitis of the hip).
Figure 1: Hip Pain - Hip Bursitis, Hip Tendonitis - Physio Frenchs Forest, Physio Macquarie Park
What are the signs and symptoms of glute med tendinopathy?
If you are suffering from gluteal tendinopathy (hip bursitis), you are likely to be experiencing:
Point tenderness over the greater trochanter (the large bony protuberance on the outside of the femur)
Pain that can refer from the hip into the outside of the thigh
Lateral hip pain (pain on the outside of the hip) that worsens with certain activities (e.g. climbing stairs, running)
Pain with prolonged sitting, or when sitting with legs crossed
What causes glute med tendinopathy?
One of the main causes of gluteal tendinopathy is the weakness of the gluteal muscles themselves, which for biomechanical reasons can end up with greater compressive forces being placed on these tendons
Due to anatomical variances, gluteal tendinopathy is more common in females than in males
The presence of gluteal tendinopathy can display a strong association with obesity, due to the increased biomechanical forces placed on the tendons of the hip
Gluteal tendinopathy is most commonly seen in patients aged between 40 and 60 years old
Training/load errors are also flagged as a major cause of gluteal tendinopathy, whether this be due to a dramatically increased training load, or a change in surface that the training takes place on
What Physiotherapy exercises help glute med tendinopathy?
Your physiotherapist will suggest a number of strategies to firstly reduce your pain, and then slowly build the tolerance/strength of your hip musculature, over a number of weeks.
Activity modification is an important part of the treatment for gluteal tendinopathy. Reducing your training load to an appropriate amount is likely the first step your physiotherapist will make. They will also ensure that you are avoiding any provocative activities. Patients should reduce their walking load and avoid running, limit the use of steps and hills, and finally avoid sitting on the floor cross-legged.
Over the first few weeks of your treatment plan, your physiotherapist will likely perform manual therapy of the muscles and joints surrounding your hip, in an effort to reduce your pain and increase your ability to participate in your chosen activities. They will also prescribe you with a home exercise program, that aims to progressively build up the strength and endurance of the hip musculature, to ensure long term resolution of your symptoms.
See our expert Physiotherapy team at Frenchs Forest and Macquarie Park!
References:
Fearon AM, Scarvell JM, Neeman T, Cook JL, Cormick W, Smith PN. Greater trochanteric pain syndrome: Defining the clinical syndrome. BR J Sports Med. 2012;0:1-5.
Lin CY, Fredericson M. Greater Trochanteric Pain Syndrome: An Update on Diagnosis and Management. Curr Phys Med Rehabil Rep. 2015:3(1);60-66.
Speers CJ & Bhogal GS. Greater trochanteric pain syndrome : a review of diagnosis and management in general practice. BR. J. Gen. Pract. 2017;67(663);479-480.